Written by James Lyons
James Lyons is a registered clinical nutritionist with special interest in preventative medicine, endocrine conditions and LGBTQI health. He is passionate about health education and patient autonomy, and he supports resources that empower everyone to make informed decisions about their health. James lives in the eastern beaches area of Sydney, Australia and works globally.
Iron deficiency is the most frequent nutrient deficiency and the most common health problem in the world.
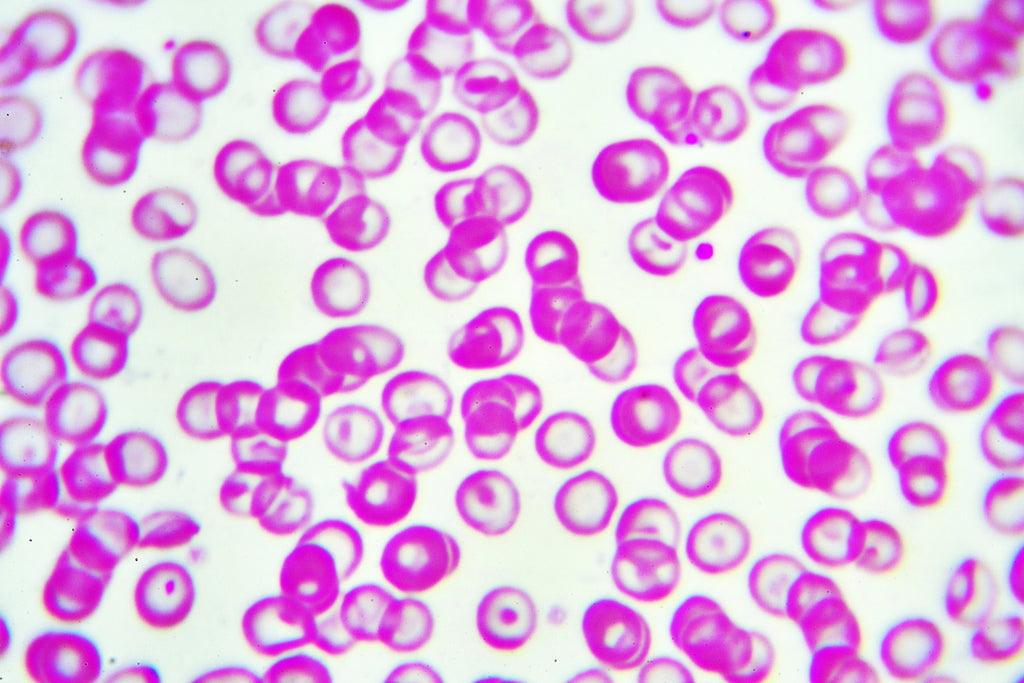
Iron is a trace element that is essential for the synthesis and function of haemoglobin, a protein found in red blood cells that carries oxygen throughout the body. Low levels of iron cause red blood cells to contain poorly formed or completely missing haemoglobin, leading to impaired oxygen delivery and anaemia – a condition of inadequate oxygen supply to cells throughout the body. Haemoglobin is like a long, wriggly ribbon bunched up inside the red blood cells. Attached to the “ribbon” are iron ions – these are what the oxygen ions attach to. Without iron, haemoglobin just doesn't work.
Iron is also required for a strong immune system, mood stability, cognition and mental health, DNA synthesis, cell division and all stages of growth.
Causes of Iron Deficiency
Risk Factors for Iron Deficiency in Adults:
- Blood Loss. Red blood cells contain a lot of iron and losing any blood can deplete the body's iron stores quickly. Blood loss may be due to bleeding disorders, frequent nose bleeds, heavy or irregularly frequent menstruation, surgery (including giving birth), blood donations, or undetected bleeding from gastrointestinal disorders or use of some over-the-counter pain relievers such as aspirin or ibuprofen.
- Insufficient Diet. Iron is an essential nutrient, meaning that the human body needs to get it from food. Vegetarians and vegans need to keep an eye on their iron intake, as the highest levels of iron are found in meat and other animal products. But maybe the rest of us could learn something from the vegans – a 2016 prospective study found that they had higher intakes of iron than meat-eaters.
- Absorption Issues. The intestines absorb iron from any food you eat and transport it into the bloodstream. Any gastrointestinal disorders affecting the small intestines (e.g. coeliac disease) can stop the absorption of iron, eventually leading to a deficiency. Other issues with digestion can also affect iron levels. Stomach acid is required to free iron from protein-rich foods like meat during digesting. Without adequate digestive fluid, iron remains trapped in the food and excreted through the bowels. There are a number of reasons for low stomach acid – most commonly, it naturally decreases as we age.
- Increased Need. Iron requirements change throughout the lifespan – any time of increased growth and development demands a high amount of iron. Pregnancy and breastfeeding use a lotof stored iron, as do growth spurts and body-building. Endurance activities like marathon running and long-distance swimming also eat up iron stores and can even initiate the premature break-down of haemoglobin.
Additional Risks Factors for Iron Deficiency in Children:
- Mother with low iron levels during pregnancy and/or breastfeeding
- Low birth weight
- Premature birth
- High intake of cow's milk before two years of age
- Unbalanced vegetarian or vegan diet
Additional Risk Factors for Iron Deficiency in Teenagers:
- Extreme or sudden growth spurts
- Onset of menstruation
- Fad diets and restricted eating
- Unbalanced vegetarian or vegan diet

Weakness & Fatigue
Fatigue is a common symptom of iron deficiency, with or without anaemia. Iron is needed to “hold” the oxygen molecules in the haemoglobin found in red blood cells. With insufficient iron, there orthe blood cells don't deliver enough oxygen to tissues throughout the body. Almost all cells in the body require oxygen to create energy. This is particularly true of the brain, which utilises over 25% of the body's total oxygen consumption– more than the skeletal muscles, skin, and liver.
But fatigue can be hard to define, and it can feel different to everyone. Here's what fatigue could look like:
- Having difficulty waking up or getting up in the morning no matter how much sleep you had.
- Tiredness after any type of exertion, including walking, showering, or carrying groceries.
- Feeling lethargic, like it is an effort to do anything, including getting up out of a chair.
- Feeling like it's too much effort to socialise or interact with others.
- Fatigue usually has a gradual onset.
Weakness is different to fatigue, but they tend to go hand-in-hand in iron deficient anaemia (but not always). Weakness has more to do with a lack of oxygen delivery to the skeletal muscles, resulting in a deficit of cellular energy. Weakness can feel like:
- Difficulty lifting things that used to be easy, or that other people can easily lift (e.g. bags of groceries).
- Feeling like you have pushed yourself physically (e.g. the feeling after going on an extra-long hike) even when you have been sedentary.
- Muscle soreness that isn't improved with stretching.
- Poor grip strength. You may have difficulty opening jars or turning stiff doorknobs.
Weakness and fatigue can be caused by many situations and acute health conditions that go away on their own but tell your doctor or medical team if you experience weakness or fatigue for over 2 weeks – it could be due to an iron deficiency.
NOTE: While weakness and fatigue are the most common symptoms of iron deficient anaemia, some people can have an iron deficiency without developing these symptoms at all. The following symptoms may occur without any feelings of fatigue or weakness:
Shortness of Breath
Huffing and puffing just walking down the street? Feel like you can't take a deep enough breath? Shortness of breath could be due to an iron deficiency. When there is an insufficient amount of iron to carry oxygen through the body, the lungs have to work overtime to load up any available iron with oxygen.
NOTE: Some people with iron deficiency experience chest pain instead of shortness of breath.
Hair Loss
Hair follicles need to create cellular energy, too. When they are deprived of oxygen, a hair follicle will move into its “telogen phase” – this is where no new hair is being made and the existing hair is released from the follicle. Normally, the telogen phase is followed by an active “anagen phase” where cells are dividing rapidly, creating a thick, new hair shaft. But this cellular division and follicle activity requires a lot of iron to carry oxygen to the site, andas part of the building material for the hair shaft. Without enough iron, the hair simply falls out and doesn't grow back until iron stores are restored.
While iron deficiency is typically only associated with unusual, patchy hair-loss, recent research suggests that low levels of iron may also speed up age-related pattern baldness in both men and women.
Body Signs of Iron Deficiency
Red, Smooth, Swollen Tongue Iron deficiency can make your tongue look shiny, red and puffy – this is called glossitis. The surface of the tongue becomes smooth and shiny when there is a lack of oxygen delivered to the mouth tissue, resulting in inflammation and redness. If the anaemia continues, the tongue may continue to swell and cause difficulty talking, chewing or swallowing. There may be pain, and the papillae (taste buds) on the tongue may disappear – don't worry, they will regrow once iron levels are restored to a healthy level.
Pale Palms and Creases Pale skin is a common sign of iron deficiency anaemia, where there are insufficient red blood cells to flush the skin with pink hue. The easiest way to see this pallor is on the palms of the hands. If you're unsure what constitutes “pale”, check out the lines of your palms. These are known as “palmar creases” and because these crevices are thinner than the rest of the skin of the palm, they are more translucent and closer to the vascular system. Normally, when you stretch your palm these creases will appear pink or light red. In iron deficiency anaemia, they'll remain the same pallid shade as the palm, or a very pale pink.
Pale Conjunctiva The conjunctiva is a thin membrane that covers part of the front of the eye and the inside of the eyelids. It is clear and covers a the highly vascular eye tissues that have strong blood supply. To check for iron deficiency, look in the mirror, gently pull down your bottom eyelid and check out the colour of the conjunctiva lining the lid. Normally, the inside of the eyelid is a distinctly flushed with a rich, red-ish pink colour that is different to the white-ish pink of the eyeball. In iron deficiency, it may appear a pale pink, or even white.
Mood Swings, Depression & Anxiety
Feeling run down and weak is bad enough, but recent research has shown that low iron levels may contribute to serious mood issues and conditions like depression and anxiety. A 2018 study of 1,000 adults found a significant correlation between iron deficiency and history of depression.

Iron is an essential cofactor in the synthesis of neurotransmitters and hormones that control mood, cognition, and mental well-being. It is also needed to maintain myelin, the protective membrane that lines nervous tissue – without myelin, nerves can fire incorrectly and send mixed up signals.
Studies have found that having low iron levels significantly decreases the amount of adrenaline and noradrenaline found in the brain, leading to feelings of apathy and “low arousal” – nothing can get you up and going. It has also been linked to low levels of serotonin, the “happy” chemical that is also responsible for motivation, interest, appetite, libido and sleep.
Children and teens are particularly susceptible to the mood and cognitive symptoms of iron deficiency, as their nervous systems and brain tissues are still growing – a process that demands high levels of iron. Depression during pregnancy has recently been linked to low levels of iron in a retrospective study of 142 patients. The study demonstrated that the odds of developing depression were 2.5x higher in pregnant women with an iron deficiency than those with healthy iron status.
Other neurological symptoms caused by iron deficiency can include:
Frequent Infections
Iron is a fundamental element for healthy development and maintenance of the immune system. As a component of DNA replication, it is needed for the growth and health of immune cells, and it is a co-factor in many immune reactions. Iron deficiency impairs all levels of immunity, from the front-line barriers of the mucus membranes in the sinuses, mouth, throat and digestive system, through to the white blood cells that attack pathogens throughout the body. Several studies have shown links between low iron status and frequency of acute infections.
There's an important caveat here – not everyone with an iron deficiency will experience frequent infections. Here's why – some pathogens loveiron and will steal it from the host in order to survive. In some cases, severe iron deficiency can actually be protective against infections, and illness may not take hold for long simply because there is not enough iron for pathogens to survive. If you are sick and iron deficient, taking an iron supplement may actually feed these pathogenic microorganisms, making the infection even harder to shake. Seek medical advice before beginning iron supplementation during or after an infection.
NOTE: Some infections can even mask an iron deficiency in blood work. The inflammation caused by feverous infections increases the number of iron carriers in the blood, which lookslike there is more iron but really there are only more carriers. One study suggests waiting at least one month after a fever before relying on blood work to accurately assess your iron levels.
Iron Deficiency in Children & Teenagers
Iron is needed for cell division and many stages of growth in all types of body tissue. Children and teenagers with low iron may show these additional signs of iron deficiency:
- Growing slower than expected
- Loss of appetite
- Eating dirt or other non-food items
- Poor co-ordination and motor skills
From embryonic development through to adulthood, iron is essential for brain growth, the development of the microstructures of the brain (e.g. blood vessels and nerves), and the synthesis and balance of signalling chemicals and hormones. A deficiency of iron during stages of development and growth can lead to a range of issues, from mild social difficulties through to severe cognitive dysfunctions.
Iron deficiency can present in children and teenagers can also look like:
- Behavioural issues
- Poor attention span
- Prolonged effects on behaviour and development milestones
- Children with anaemia may be less active and timider than their peers
Correcting an Iron Deficiency, The Right Way
An iron deficiency can be confirmed through a blood test. Haemoglobin level is a key indicator of iron status, and the normal ranges for adults is 12.0 – 17.5 g/dL. Anything below this may cause symptoms of anaemia. Your doctor can also check the size, shape and concentration of red blood cells through a blood test.

Specialised iron studies include checking for ferritin (the protein that stores iron the body), transferrin (transports iron around the body) and transferrin saturation (an indicator of how much iron is actually bound to transferrin).
Correct the Underlying Issue
Most causes of iron deficiency are diet-related, but many cases involve undiagnosed medical conditions. To successfully treat an iron deficiency, it is essential to first identify the underlying reason why iron levels are low and to treat the cause. While undergoing treatment, your medical practitioner or nutritionist may recommend boosting your iron levels through diet or supplementation.
Iron from Food
Dietary iron is found in one of two forms in foods: heme and non-heme. Heme iron is the type of iron found in haemoglobin (a part of red blood cells) and is therefore found in animal products like meat, fish and poultry. About 50% of iron found in these sources is heme iron. The remaining 50% is non-heme iron.
Non-heme iron is mostly found in plant foods such as nuts, fruits, vegetables, grains and soy products. Dairy contains a little non-heme iron but is considered a poor source of iron. Some breads, pastas, cereals and flours have been fortified with iron.
Non-heme iron has to be converted into heme iron before the intestines will absorb it into the body. This conversion happens in the gastrointestinal tract with the help of stomach acids and other digestive fluids. Sugar, particularly fructose, and vitamin C can enhance this process and improvethe digestion and absorption of non-heme iron by up to 75%.

TIP: Avoid including calcium-rich foods such as milk, cheese or yoghurt with your iron-rich meals. Calcium inhibits iron's absorption.
Mild iron deficiencies may be resolved by incorporating iron-rich foods into the daily diet. These include:
- Beef (85g = 2.2mg)
- Chicken (1 cup = 1.8mg)
- Curly leaf parsley (1 cup = 1.9mg)
- Tempeh (125g = 11.5mg)
- Tofu (125g = 3.7mg)
- Quinoa (1 cup = 2.8mg)
- Lentils (1 cup = 5.2mg)
- Chickpeas (1 cup = 3.6mg)
- Spinach (1 cup cooked = 6.9mg)
- Silverbeet (1 cup cooked = 3.9mg)
It can be quite difficult to remedy a moderate to severe iron deficiency with diet alone. Your nutritionist or doctor may recommend iron supplementation.
How to Use Iron Supplements
Iron supplementation is usually a quick and effective way to treat an iron deficiency – but there is a catch. Iron is toxic in high doses and can cause serious damage when it accumulates in the body. Taking iron supplements unnecessarily, or for longer than needed, can lead to iron overload and increase the risk of developing diabetes, heart failure, arthritis, liver disease and hormone issues. Keep in mind that symptoms of an iron deficiency may actually be caused by a number of different conditions and speak to your health practitioner before taking iron supplements.
Cautions & Contraindications
Iron supplements can be dangerous if you have:
- Haemochromatosis
- Anaemia without iron deficiency
- Iron malabsorption
- Infectious intestinal diseases (e.g. parasites, pylori)
- Diverticular disease or ulcerated colon
- Untreated infections
Once you have a confirmed diagnosis of iron deficiency, its underlying cause and an all-clear from your medical team, you can begin taking iron supplements. They are available as liquids (including Nu U Nutrition Liquid Iron supplement), tablets, capsules and powders and often contain vitamin C to improve their absorption. It is important to take your iron supplement daily, or as prescribed, to provide the body with a steady supply. Many people feel improvement in iron deficiency symptoms within 2 weeks of taking iron supplements – but it is important to continue taking the supplements for as long as your nutritionist or doctor has prescribed.
TIP:If you are prone to constipation, take an enteric coated iron supplement – other forms are notorious for slowing down the bowels.
CAUTION
Too much iron can lead to toxicity, diabetes, liver damage, hormone dysfunction and heart failure. Use only as directed. Speak to a qualified nutritionist, naturopath or doctor for personalised advice.